CDC Report: Why Do Certain Populations Never Screen for Colorectal Cancer?
Cancer screening remains a powerful tool. Even limited screening has long-term benefits compared to no screening and can lower the risk of cancer and related deaths. A recent study by researchers at the CDC compared data on adults who reported they had not received a colorectal cancer (CRC) screening test between 2012 and 2020 using information from the Behavioral Risk Factor Surveillance System (BRFSS). The study identified various trends, most notably that 22 states did not meet the CDC’s Healthy People 2020 goal of 70.5% adults screened for CRC.
The sample was limited to adults aged 50 to 75 years, with up to date screenings defined as one of the following:
- Home stool-blood test within the past year
- Sigmoidoscopy within five years with fecal occult blood test or within one year with fecal immunochemical test
- Colonoscopy within ten years
The ‘never screened’ numbers were a composite of those who answered no to being screened or those who were not up to date. Those who declined to answer or reported uncertainty were excluded. Overall, the study identified:
- A 5.8% decrease in unscreened adults between 2012 and 2020
- States with the largest improvements were also those with the largest unscreened population in 2012
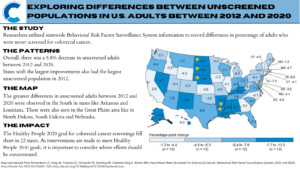
Despite these improvements, CRC screening goals have yet to be met and may be difficult to meet with the new Healthy People 2030 standards. The target of 74.4% screened may have been a challenge to meet, possibly further exacerbated by the COVID-19 pandemic.
Researchers noted that including just two more questions on the BRFSS in 2020, the percentage of up to date screenings increased to 71.6%. These two questions enquired about:
- Stool DNA testing
- Computerized tomographic colonography
It is important to note that the National Colorectal Cancer Roundtable—a membership organization established by the CDC and the American Cancer Society—has set its goal to 80% screening rates across the country.
Study authors recognized recall bias and an inability to distinguish between screening versus diagnostic tests as major study limitations. Additionally, social desirability bias and a low response rate may have also affected the results. However, financial factors and health disparities may also describe the differences between states.
Following implementation of the Affordable Care Act, researchers at the American Cancer Society found that CRC screening among low-income adults across the U.S. increased by up to 8%, with the greatest increases observed in early Medicaid expansion states. They also noted that a majority of those who were never screened also lived in a state without expansion (South Dakota).
Nonfinancial factors such as health disparities were studied in a mixed-methods analysis conducted at the Virginia Commonwealth University’s School of Medicine. Here, researchers noted that participants of gender-specific and race-specific focus groups brought forth nuanced concerns regarding screening. This included lack of awareness of both the disease and the screening, lack of physician recommendation that is clear and rational, and fear of being diagnosed and complications associated with testing. These concerns, if unaddressed, may limit others from seeking out CRC screening.
To read more about the Healthy People 2030 CRC screening standards and the current progress, visit Healthy People 2030.
Kaylinn Escobar is a Colorectal Cancer Prevention Intern with the Colon Cancer Foundation.







Leave a Reply
Want to join the discussion?Feel free to contribute!