By Anna Payne
Thank you to the Cystic Fibrosis Research Institute for letting us share this blog with our audience!
Last year, at the age of 34, I was living in a place of hope. I was thriving on Trikafta, working full time, serving as elected Supervisor for Middletown Township in Bucks County Pennsylvania, and acting as Vice-Chair of the Pennsylvania Rare Disease Advisory Council. For the first time in a long time, I had hope for a future of a “healthy” life. I had big dreams and a lot of things I wanted to accomplish. But then I found a mass in my groin, and after a long, painful and circuitous diagnostic journey, that included numerous invasive tests and long waits between them, I received the news no one wants to hear. “You have Stage 4 colon cancer.”
Known as the “silent cancer,” colorectal cancer remains the third leading cause of cancer-related deaths in the U.S. among the general population. Those with cystic fibrosis have a significantly higher risk of colon cancer than the general population. For those with CF who have not had a transplant, their risk of colon cancer is five to ten times higher, while individuals with CF post-lung transplant have twenty times the risk as the general population.
What makes us especially vulnerable is that colon cancer symptoms can and often do mimic issues that we CF survivors experience daily. More research is needed to determine exactly why we’re at such elevated risk for the disease, but it’s believed to be linked to a mutation in the cystic fibrosis transmembrane conductance regulator (CFTR) gene.
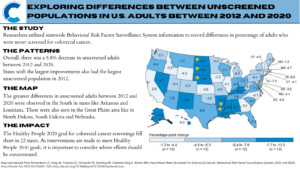
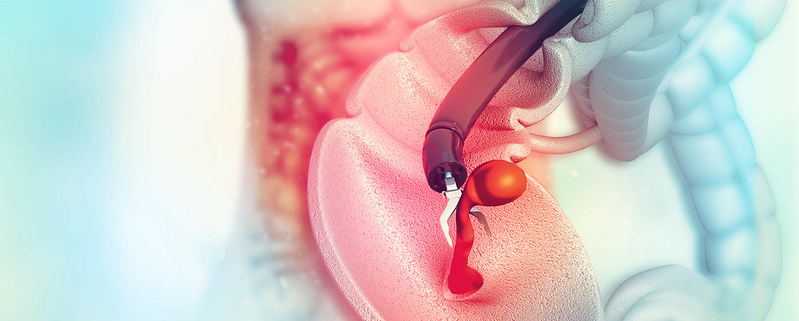
The most effective tool for preventing this silent disease is a colonoscopy. Colon cancer always starts in the form of polyps, which if found early can be removed prior to becoming malignant. Colonoscopies are recommended for the general population at 45, yet despite our highly elevated risk, the current recommendation for a first screening colonoscopy for a person with CF is 40. That’s too late and must change. Screenings can prevent about 60 percent of colorectal cancer deaths.
I was 34 years old when diagnosed; I had few symptoms and no known family history. Colon cancer grows slowly, and it’s possible it’s been in me for years. I initially sensed that something was wrong when I had minor digestive issues. They persisted, but I second-guessed myself. Then I found a mass in my groin about the size of a dime.
After an inconclusive ultrasound, and while waiting for an appointment with a general surgeon, the lump grew to the size of a walnut. I went to my CF team for help. They found a bowel blockage, a common condition for those with cystic fibrosis known as Distal Intestinal Obstruction Syndrome, or DIOS. We hoped a colon cleanse would clear the blockage, but deep down I knew it was something more serious.
After a CAT scan and a biopsy of the groin mass, came the bad news. Cancer. I burst into tears. A PET scan then revealed the cancer had spread to other organs, including my ovaries, liver – which had 14 lesions – and lymph nodes.
After thriving on modulators, I have been transformed by cancer back into that sick, little vulnerable girl with CF who spent many nights curled up in a hospital bed, unsure of her future. I am now undergoing aggressive chemotherapy, requiring me to be outfitted with a take-home pump. Five times a week, I’m hooked up to an IV pole at home, on fluids to help me re-hydrate. Chemotherapy leaves me fatigued and immunocompromised, susceptible to infections and viruses that can be deadly.
Naturally, that’s required me to adjust my social life, relying on a network of friends. Work has taken a backseat to the battle at hand, but my supportive employer allows me to work remotely — as much as I’m able. My wonderful colleagues have carried the load in my absence. I miss them. I’ve even come to miss the 45-minute commute to my office with a stop to get a hot tea at Dunkin’.
Simple joys like eating — which most of us take for granted — are now a chore. I eat for calories, not pleasure. My diet changed drastically, and I no longer enjoy foods I’d grown up eating, such as macaroni and cheese and steak. If you looked in my cabinets now, you’d mainly find massive amounts of Fruit Loops and Apple Jacks.
I was shocked when my platinum blonde hair – with blue streaks – fell out in clumps. Losing hair is traumatic – it’s about body image, one’s sense of self, and feeling normal. Many have told me not to worry, that it will grow back, but I have no idea how long I will be on chemo, and whether that is true. While I have multiple wigs that allow me to feel like a different superstar each day, and a wide array of knitted hats, I often scrap these so I can emulate my idol, the Rock.
As a little girl, I spent a lot of time inpatient at St. Christopher’s Hospital for Children in Philadelphia. Watching the Rock on the weekly Smackdown was a great escape. Amazingly, the Rock learned about my diagnosis and sent me a heartfelt video wishing me luck in my fight. It’s been viewed millions of times on his Instagram page, and has allowed me to feel less isolated, with a virtual connection to countless people who channel their positivity toward me.
Prior to my diagnosis with colon cancer, I planned to travel across the globe. I wanted to hold a koala bear in Australia and visit Costa Rica. I planned to run for higher elected office. I had hopes and dreams that have been put on pause. I live in a world of uncertainty. Once again, I am learning to be comfortable living in the uncomfortable.
As science improves and evolves, so should our thinking. Cancer screenings must become a normal routine for cystic fibrosis adults, and the sooner the better. My hope is that the recommended age for a first colonoscopy will be lowered to 25 years for those with CF.
But you don’t have to wait for that to happen. If you have symptoms, don’t write them off as the usual CF GI issues. Go and get screened. You may end up saving your own life.