By Parker Lynch
According to the Mayo Clinic, cystic fibrosis (CF) is a disorder in which there is severe damage to the lungs and other organs in the body. This condition presents itself differently in each patient when comparing manifestations of symptoms; however, wheezing, difficulty breathing, exercise intolerance, constant lung infections, and recurrent sinusitis are all very common among individuals with CF. People with cystic fibrosis are very strong and admirable, as their condition can be very arduous in terms of treatment and monitoring: the need for consistent medication (bronchodilators, mucus thinners), using special devices and techniques to assist with breathing, monitoring what they eat, etc.
Though it seems like CF and colorectal cancer (CRC) wouldn’t even be remotely related, adults with CF actually have a 5-10 times higher risk of developing CRC as opposed to adults without CF. On top of this, individuals with CF who receive lung transplants (or any other solid organ transplant, for that matter) are 20 times more likely to develop CRC, which requires them to complete their preventative screenings at the age of thirty rather than the standardly-recommended age of forty-five.
You can read about a CF patient’s experience with her surprise diagnosis of CRC.
Where is This Connection Coming From?
As with any other condition or diagnosis, researchers aren’t completely certain of what the singular cause is of a CF patient’s higher chance of developing CRC. However, it is believed that mutation in the cystic fibrosis transmembrane conductance regulator (CFTR) gene may have a role to play. Mutation in the CFTR gene not only leads to the development of CF, but can also lead to the development of CRC, though more research needs to be done on this topic to be able to analyze the strength of the correlation between the two.
Moving Forward With This Information
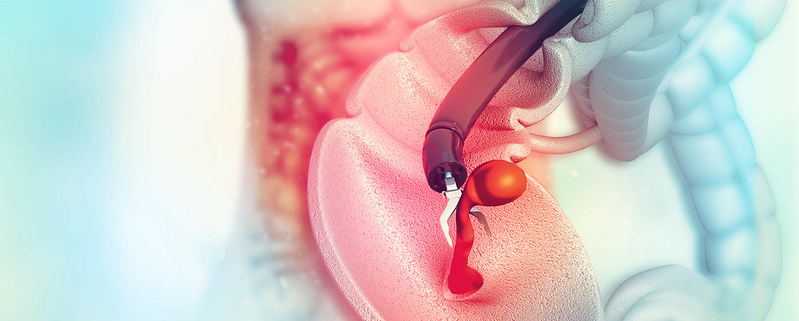
Patients with CF are recommended to receive regular colonoscopies beginning at the age of 40 (which is five years younger than typically recommended among the adult population). Those who have received lung transplants are recommended to get their screenings at the age of 30, due to the aforementioned risks that come with organ transplantation and CRC development.
Outside of preventative screenings, monitoring CF and CRC requires collaborative efforts among different healthcare providers as well as the individual themselves. The important factor here is that CF patients are made aware of their increased risk of getting CRC, and have a support system in navigating appointments, physician communication, screenings, etc.
Monitoring one condition alone is extremely stressful and taxing on an individual, let alone having to deal with two. The American Cancer Society has a list of psychosocial resources for individuals who need support with navigating their healthcare, while also helping provide financial assistance, individual therapy, and group therapy. Health concerns are never easy to deal with, and it is always okay to reach out for help.
Parker Lynch is a Colorectal Cancer Prevention Intern with the Colon Cancer Foundation.
Image credit: Gordon Johnson from Pixabay