Regular screening, surveillance, and high-quality therapy can help prevent colorectal cancer (CRC) incidence and mortality. However, a lot of people put off being tested for a variety of reasons, including:
- Hearing from others that the test could be challenging or uncomfortable and that talking to their doctor about CRC or handling feces could be embarrassing
- In the absence of a family history of CRC, they believe they are not at risk and don’t need to be screened
- Cost of getting tested
- The complexity associated with screening, which could include out-of-pocket costs, taking time off work, and transportation to the clinic
Here’s information on the different types of screening options for CRC.
Blood Tests Are Emerging as a Potential Screening Option
While legitimate, these concerns have over time created obstacles to CRC detection at an early stage, when the cancer is easier to treat. But, alternative options are being developed that do not require handling stool samples or undergoing a colonoscopy (which may need time off from work), such as blood-based testing.
A study that was recently presented at the annual meeting of the American College of Gastroenterology, found that patients who were given the option to undergo a blood-based CRC screening test were more than twice as likely to finish the screening process than those who were given the stool-based option.
Of the 1,927 eligible study participants, 924 were assigned to the blood draw group and 1,003 to the stool-based testing group. More than 50% of participants in the blood-draw group made an appointment with the research team after they were contacted by phone. After three months, CRC screening was 19.4% higher in the blood-test group than the stool test group (32.4% vs. 13.0%).
Traditional CRC Screening Options
Traditionally, the following screening options have been use for those with an average risk of CRC (meaning no family history of polyps of CRC or personal history of polyps or CRC):
- Fecal immunochemical test (FIT) test is performed annually
- FIT-DNA test is performed every three years
- Guaiac-based fecal occult blood test (gFOBT) is performed annually to screen for CRC
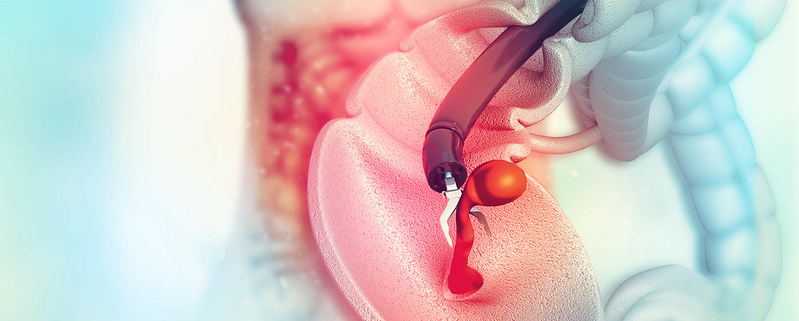
- Colonoscopy is performed once in ten years
The FIT and gFOBT tests are at home and require a small bit of stool sample to be collected with a stick or brush and sent to a laboratory for testing. On the other hand, a whole bowel movement is taken for the FIT-DNA test and sent to the lab to be examined for altered DNA and the presence of blood.
A colonoscopy is a little more complicated in that it requires some preparation the previous day and anesthesia during the procedure.
On the contrary, extracting blood may be less painful, awkward, or time-consuming. Blood-based tests for CRC can have several benefits and lower testing barriers. Nevertheless, patients need to be properly informed of their options, and more research is required to gauge the extent to which blood tests for CRC are effective and comparable to other screening options in detecting cancer.
Emmanuel Olaniyan is a Colorectal Cancer Prevention Intern with the Colon Cancer Foundation.