There are two kinds of health literacy: personal health literacy and organizational health literacy. Personal health literacy describes the extent to which people have the capacity to locate, comprehend, and apply information and/or services that they have obtained to make informed health decisions and actions for themselves and others. Organizational health literacy is the extent to which organizations and associations equip individuals with what is necessary to draw conclusions and inferences that enhance their understanding and enable them to make informed health decisions and act for themselves and others.
Why is Health Literacy Important?
Health literacy is instrumental in influencing health disparities because it can serve as an essential barrier or bridge to comprehension of health education material. An impactful determinant of health, a person’s health literacy is more likely to accurately predict their behaviors when compared with economic status, age, or ethnic background. Health literacy also has a substantial effect on an individual’s health: those who lack health literacy are twice as likely to be hospitalized as those who possess satisfactory levels of health literacy. The most common cause for this could be: misinterpretation of information or incorrect dosage of self-administered medication or treatments.
Those who lack health literacy may be ashamed and/or hesitant to open up about this issue with their healthcare providers for fear of judgment, and this may hinder their trust in the healthcare industry. This in turn may be pernicious towards their overall well-being.
How Can We Account for This When Developing Educational Materials?
There are an abundance of ways to make accommodations in health resources in order to account for differences in health literacy.
- Use Plain Language
-
-
- Avoid technical slang or jargon
- If technical terms are used, be sure to define them in lay language and contextualize it so that the intended audience understands how and when it is utilized.
- If the health resource is an article, include a plain language summary (this is something that the database Cochrane practices), a glossary of terms and words with phonetic pronunciation guides, and at least one example of how the term or phrase is used.
- Avoid technical slang or jargon
-
- Be Aware of Appropriate Phrasing and Preferred Communication
-
-
- Be sure to provide materials in the languages that are most often spoken in your area, and to interact with reliable translators to verify that the facts are coming across correctly and fully in all languages.
- Brochures, forms, and other materials at health education events can be available in multiple languages
- It is important to be aware of perception of words used in verbal and written communication
- For instance, avoid the qualifier “disorders” when discussing mental health or the term “co-morbidities”, since they carry negative connotations. Instead, opt for terms such as “mental health conditions”, and “co-occurrences”.
- Identity-first vs person-first
- Identity-first language puts a person’s condition before the person, and person-first language puts the person before their condition.
- Preferences depend on the community, so it is important to consult a variety of sources and be receptive to your audience(s) and their input.
- Identity-first language puts a person’s condition before the person, and person-first language puts the person before their condition.
- Be sure to provide materials in the languages that are most often spoken in your area, and to interact with reliable translators to verify that the facts are coming across correctly and fully in all languages.
-
- Visual Supplements for Written Materials
-
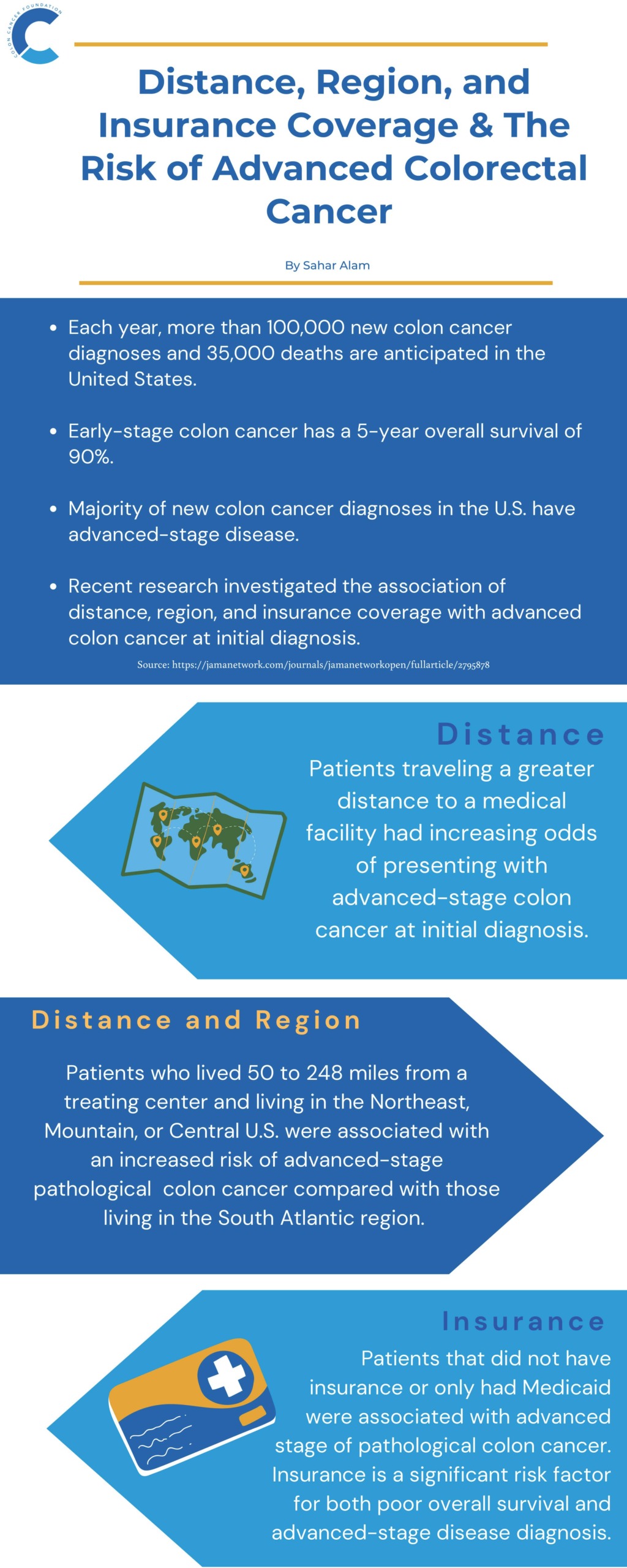
- Infographics
- Can provide helpful imagery to highlight main ideas of the research
- Assists people who may have trouble imagining what the text is conveying
- Text, Font, and Contrast
- Large text can be helpful for people with visual impairments
- Fonts should be clear and legible
- Colors, hues, or both for background and text should contrast in a way that does not obscure the information
- Infographics
Just as zip code is a salient social determinant of health, health literacy serves as an important indicator of potential health behaviors and outcomes. Being able to consume, understand, and disseminate health information will help people and those they care about immensely in that the decisions made and actions taken will be more robustly supported and informed.
Reach out to us at [email protected] if you would like to collaborate and create accessible health materials pertaining to colorectal cancer, prevention, or another related topic!
Vanessa Seidner is a Colorectal Cancer Prevention Intern with the Colon Cancer Foundation.
Photo credit: Alexander Grey on Unsplash.