By Parker Lynch
The COVID-19 pandemic has had a lot of repercussions within the healthcare realm. The inability of patients to visit their providers in-person (out of fear of COVID-19 exposure) led to the expansion and adoption of telehealth services all across the world. While we have a better handle on the pandemic in America, telehealth services are still being utilized by physicians from a vast assortment of specialties. Telehealth increased access and was beneficial to patients as well as doctors, there are some caveats.
A recent article shares how patients are now really comfortable emailing their doctor to provide health updates or ask medical questions. Patients may live several hours away from a specialist’s clinic or might be too sick, which may make it inherently difficult for them to schedule in-person appointments. Justifiably so, they might prefer to reach out to their doctors via the clinic’s or hospital’s patient portal. As a result, doctors are flooded with email messages, many of which are received after hours. Doctors feel obligated to answer all of these questions/comments, 24/7.
Patient Portal Communication Causing Physician Burnout
Due to the burnout that physicians are experiencing from this constant and overwhelming communication, hospitals including Johns Hopkins, Houston Methodist, and the Cleveland Clinic have begun charging patients for the clinical advice that they are receiving through messages. The goal of these charges is to reimburse physicians for their time, but has discouraged patients from contacting their providers.
Many doctors believe that open communication between them and their patients is vital to an accessible healthcare system and do not want their patients to ever refrain from reaching out. At the same time, these doctors also recognize that open communication can’t feasibly mean “open” 24/7. Moving forward, it is important to keep in mind that this issue is hardly black-or-white. Should patients continue to be charged for messaging their providers, there will be accessibility barriers for those that cannot afford these charges. On the other hand, constant communication between patients and their doctors has proven to be detrimental to the doctors themselves. Eve Rittenberg, a physician and professor at Harvard Medical School, believes that this line of communication should remain, with boundaries in place.
Implications for Cancer Patients
For patients in the cancer realm, specifically, there are some implications of this limited/“controversial” communication. Dr. Jyoti Patel, suggests several different ways in which patients can effectively use their patient portal messaging features. Most importantly, one should never send a message regarding chemo-induced fever or sudden symptom changes, rather they should immediately call the doctor’s office. Chat features with physicians should never be used to discuss complex questions that revolve around one’s diagnosis, prognosis, goals of treatment, etc. It can be very difficult for physicians to properly convey their thoughts on these matters. Instead, patients should only be asking questions that yield a straight-forward and easy response (like prescription refills, appointments, etc.).
Boundaries can be really hard to establish between patients and their doctors. However, the fundamental goal of wishing the absolute best quality of care for a patient remains consistent. Hopefully, a happy medium can be met: allowing the patients to communicate with their providers without the providers feeling overwhelmed.
Parker Lynch is a Colorectal Cancer Prevention Intern with the Colon Cancer Foundation.
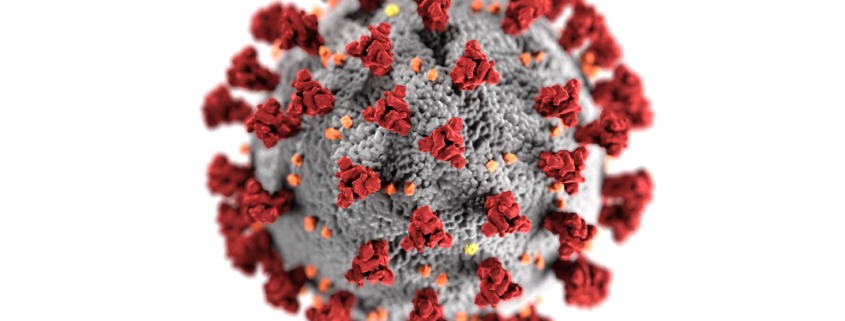
Image credit: National Institutes of Health