The Colon Cancer Foundation (CCF) is heartbroken to learn of the passing of a superhero, Chadwick Boseman. Boseman’s life was tragically cut short on August 28 after a four-year battle with colon cancer, the nation’s second deadliest and third most commonly diagnosed cancer. “On behalf of the thousands of patients, caregivers, clinicians, and researchers who we represent, the Colon Cancer Foundation would like to offer our sincerest condolences to the Boseman family and our support to the millions of people who were touched by Chadwick.” said Cindy R. Borassi, Interim President.
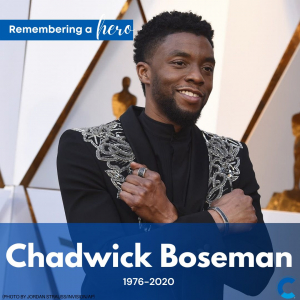
Chadwick Boseman inspired generations through his singular performances in films such as 42, Marshall, and, of course, the Oscar-nominated Black Panther. Only after his death did the world learn that he was diagnosed with colon cancer in 2016, the same year he debuted as King T’Challa in Marvel’s Captain America: Civil War. Everyone who watched him on screen knew that Chadwick Boseman was an outstanding actor. Many people also knew he was a social justice advocate and an amazing role model. Now we realize that he was also a real-life superhero, showing us what we are capable of achieving no matter what the circumstance.
Chadwick Boseman’s death tragically demonstrates the alarming increase in the rate of young people between the ages of 20-49 being diagnosed with colorectal cancer. Since 2014, CCF has hosted our annual Early-Age Onset Colorectal Cancer (EAO-CRC) Summit, the nation’s only interdisciplinary event that brings together leading clinicians and scientists, as well as EAO-CRC survivors and caregivers from across the globe. The program provides extensive opportunities for participants to advance their understanding of the rapidly increasing incidence of CRC among young adults under 50 years of age in the U.S. and abroad. We encourage you to check out the executive summaries of our past Summits to learn more about EAO-CRC: https:/eaocrc.org
Boseman said in a 2018 interview, “You should be the hero in your own story.” The Colon Cancer Foundation has been encouraging people to be their own heroes and heroines since 2008 by raising awareness and spreading the word that colorectal cancer is treatable and beatable with early detection and screening.
As we continue to work towards A World Without Colorectal Cancer™, we encourage you to “be the hero in your own story” and #CheckItForChadwick. To donate in Chadwick’s memory using the following link: https://ccfdonations.greatfeats.com/donate

