Often, colorectal cancer (CRC) doesn’t cause symptoms until it grows or spreads. It is often harder to detect in the younger population who might ignore symptoms due to lack of insurance coverage, and because they are not yet eligible for screening because of their younger age. However, findings from a recent study might provide some clues to identifying the early onset of CRC among young adults not old enough to qualify for CRC screening.
Those under 45 may not have insurance coverage for any form of CRC screening—colonoscopy, FIT, or FOBT—because the recommended age to start screening for CRC is 45 years. According to the American Cancer Society, 2,001,140 new cases of cancer are projected in the U.S. in 2024,152, 810 of which may be CRC. Another concerning statistic is the 2% rise in the annual CRC incidence rate among young adults (ages <55 years).
Paying Attention to The Early Signs
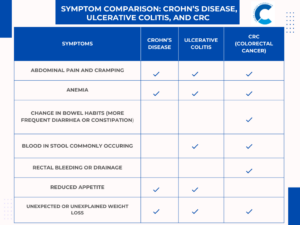
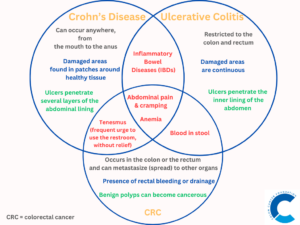
The study identified 4 red-flag signs and symptoms occurring at least three months before diagnosis that were associated with a subsequent risk of early-onset CRC:
- Abdominal pain
- Rectal bleeding
- Diarrhea
- Iron deficiency anemia
A total of 5,075 early-onset CRC cases and 22,378 controls were included in the study. 63% of the cases were diagnosed with CRC. The authors found that in the study population:
- Abdominal pain and rectal bleeding were the most common symptoms
- Abdominal pain was associated with a 34% higher risk of early-onset CRC
- Signs of rectal bleeding had the greatest association with developing CRC
Diarrhea and iron deficiency anemia were also identified as a common symptom but did not have a high association with CRC.
Having one, two, or three of these warning signs and symptoms were linked to a 1.9-, 3.6-, and 6.5-fold higher risk of developing CRC, respectively. These correlations were stronger for rectal cancer and young-onset cases (average 43 years).
Despite the possibility that this study helped focus on the early warning signs and symptoms of CRC, it is crucial to remember that the signs and symptoms described above can also be the result of other health conditions such as inflammatory bowel disease, hemorrhoids, irritable bowel syndrome, or infections. In order to properly identify and treat the condition, it is important to see a doctor and get screened if you are experiencing any of those symptoms.
Emmanuel Olaniyan is a Colorectal Cancer Prevention Intern with the Colon Cancer Foundation.
Picture credit: Muhammad Daudy on Unsplash