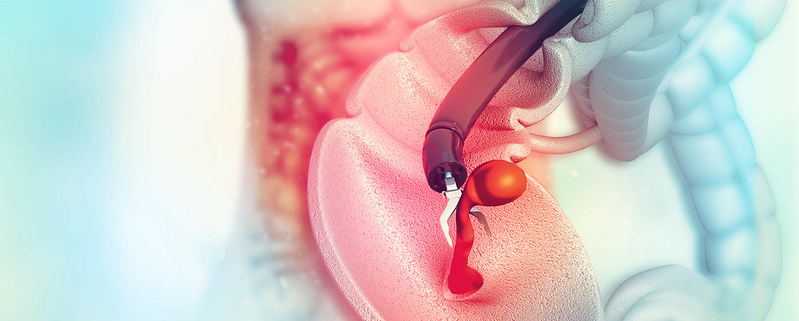
In May 2021, the US Preventive Services Task Force (USPSTF) revised the colorectal cancer (CRC) screening age for average-risk adults to 45 years. However, stakeholders are concerned about the lack of awareness, access, and motivation among the younger age group to get screened. Now, a new research study has found that the prevalence of CRC screening remained lowest for individuals ages 50 to 54 years old and young adults (age<50) experienced smaller increases in screening prevalence over time, regardless of race, ethnicity, education, income, and insurance coverage.
An investigation using population-based data from the National Health Interview Survey (NHIS), an annual, cross-sectional survey of the U.S. population conducted by the National Center for Health Statistics at the U.S. Centers for Disease Control and Prevention, studied CRC screening participation using surveys from multiple years. A sample of 80,220 participants ages 50 to 75 years old was analyzed for CRC screening participation. For each survey year, the prevalence of CRC screening was estimated for age, race, ethnicity, educational attainment, family income, and health insurance.
Racial, ethnic, and socioeconomic disparities influence screening rates. Despite the prevalence of CRC screening increasing from 36.7% in 2000 to 66.1% in 2018, screening prevalence was observed to be the lowest for:
- Participants ages 50 to 54 years old
- Hispanic populations (56.5%)
- Asian populations (57.1%)
- Participants with less than a high school degree (53.6%)
- Participants from low-income families (56.6%)
- Participants without insurance (39.7%)
This may be the result of a lack of concern for cancer and cancer screening among younger adults and their healthcare providers, limited access to healthcare, absence of or limited insurance coverage, and other priorities for young adults, such as work and family. Disparities in screening rates can potentially extend to adults ages 45 to 49 as the new USPSTF recommendations are implemented. Multilevel barriers, such as patient-, provider-, and system-level factors, impact the completion of CRC screening for young adults (age<50), creating disparities and inequities in CRC screening. The administration of new CRC screening guidelines must acknowledge and account for multilevel disparities in screening programs to ensure all populations have equal access to CRC screening and benefit from CRC screening, especially newly eligible adults ages 45 to 49 years old.
The benefits and outcomes of the updated USPSTF guidelines to extend CRC screening to ages 45 to 49 years old have been debated by clinicians and researchers. Concerns about the updated guidelines include redirecting endoscopic resources away from higher-risk and older patients, resulting in a more significant exacerbation of health disparities. Another criticism is that adults ages 45 to 49 years old who participate in screening may be less likely to belong to groups at higher CRC risk.
One benefit of expanding CRC screening to the 45-49 age group is to increase the screening participation rate among older populations. Awareness of CRC screening may also increase, resulting in newly eligible adults having more time to schedule their first screening test. However, the impact of screening among those in the 45-49 age group on disparities, benefits, and participation of older adults may take several years to be fully recognized and understood, as the USPSTF’s effect on insurance coverage only occur in mid-2022.
Sahar Alam is a Colon Cancer Prevention Intern with the Colon Cancer Foundation.








 This past February, as a CCF Champion, Suzanne and her husband were invited to attend the Cologuard Classic in Tucson, Arizona. She represented CCF and was able to meet 90 other like-minded individuals who shared her passion to make a difference and prevent early onset of colon cancer. Inspired to raise money and awareness in her hometown, Suzanne partnered with her husband’s golf club to hold a fundraising golf tournament on May 16, 2022. She was supported in her efforts by her friend, a 10-year colon cancer survivor who also works to spread colorectal cancer awareness. The event had 10 sponsors, 13 teams, and 20 hole sponsors that covered most of the costs. Half of the profits will go to their local nonprofit, CRC Life, and the other half will go to CCF.
This past February, as a CCF Champion, Suzanne and her husband were invited to attend the Cologuard Classic in Tucson, Arizona. She represented CCF and was able to meet 90 other like-minded individuals who shared her passion to make a difference and prevent early onset of colon cancer. Inspired to raise money and awareness in her hometown, Suzanne partnered with her husband’s golf club to hold a fundraising golf tournament on May 16, 2022. She was supported in her efforts by her friend, a 10-year colon cancer survivor who also works to spread colorectal cancer awareness. The event had 10 sponsors, 13 teams, and 20 hole sponsors that covered most of the costs. Half of the profits will go to their local nonprofit, CRC Life, and the other half will go to CCF.