By Parker Lynch
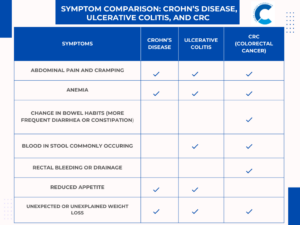
One cannot deny the importance of considering an individual’s risk of colorectal cancer (CRC) on the basis of their diet, exercising habits, and genetic predispositions. However, many other demographic factors can influence the likelihood of being diagnosed with CRC, as well as subsequent quality of life and survival outcomes.
Lower socioeconomic status, for instance, is associated with a very high risk of developing CRC. Most of these community members are uninsured, which makes it difficult for them to receive the screenings that are otherwise readily accessible for those with insurance plans. A colonoscopy (one of the most important preventative screening measures for CRC) can cost anywhere from $500 to $6,000 without insurance, depending on the site where the procedure is conducted. For those on tight budgets, paying such amounts out-of-pocket every 5-10 years (depending on their personal risk of CRC) is quite unrealistic.
Tampa Bay Study
In a retrospective study conducted in 2021 by the CDC, researchers analyzed 13,982 uninsured patients with CRC who had received services at various free clinics in the Tampa Bay area between 2016 and 2018. These patients’ demographics are as follows:
- 5,139 (36.8%) were aged 50 years or older
- Most were female (56.8%)
- A large majority were non-Hispanic White (41.1%)
- Majority were unemployed (54.9%)
Less than 7% of these patients had received any sort of preventive colorectal screening in their lives. 22.7% of these patients were smokers, and another 28.3% had diabetes. Not only are these patients more at risk for CRC because of their predisposed comorbidities, but they also don’t have the means to receive proper preventative screenings.
Bridging the Gap: Free Clinics
This study is one of many that sheds light on the healthcare treatment discrepancies among people of different socioeconomic statuses in America. The concerning statistics presented by these retrospective studies have motivated healthcare professionals and non-profit organizations to provide free clinics across the U.S. to make screening accessible to those who wouldn’t be able to otherwise afford it.
The NYC Health Department’s NYC Community Cares Project, for instance, provides free colonoscopies for uninsured residents referred from primary care sites. This program collaborates with various endoscopy centers and allows patients to work with primary care physicians, while also receiving free anesthesia and pathology services. Other interventions, such as the ColonoscopyAssist program, assists uninsured individuals in 30 states with the fees associated with CRC screening. This organization strives to eradicate a lot of the costs that are accumulated when someone gets preventative screening done, and reduces a colonoscopy’s cost to around $1,000 for a patient. Though this program doesn’t entirely eradicate colonoscopy costs, it still helps patients by significantly reducing the price, inherently making them much more feasible.
Moving Forward
These public health interventions are vital to treating patients that suffer from America’s healthcare inaccessibility issues that run rampant throughout the country. Even though the U.S. spends more money on healthcare than any other wealthy country in the world, we have struggled to match other countries in patient satisfaction, accessibility, and life expectancy.
Movements like the Community Cares Project in NYC, ColonoscopyAssist program, and other free/reduced-cost screening resources across the country are making huge strides in the CRC community. Should these endeavors continue to be subsidized by non-profit organizations, philanthropies, donations, and government support, uninsured individuals can receive timely preventative screenings. Increased access to these resources can ensure that patients from all socioeconomic backgrounds can receive the care that they need.
Parker Lynch is a Colorectal Cancer Prevention Intern with the Colon Cancer Foundation.